For veterans trying to make a compensation claim, understanding the Military Rehabilitation and Compensation Act (MRCA) is important. The MRCA supports current and former members of the Australian Defence Force (ADF) who have injuries or illnesses linked to their service. Managed by the Department of Veterans’ Affairs (DVA), it covers medical treatment, income support and permanent impairment payments.
One of the biggest concerns when submitting a claim is how long it takes. Delays can lead to financial strain, affect access to treatment, and add stress for veterans and their families. While DVA has worked to shorten wait times, there are still a number of things that can hold up a claim. Knowing how the process works—and what slows it down—can help you prepare and avoid unnecessary delays.
Key takeaways
- Complete medical records, service history and personal statements are essential for avoiding slowdowns.
- Initial Liability claims now average around 100 days, while Permanent Impairment claims sit around 227 days.
- Claims that involve multiple conditions or require extra medical assessments naturally take more time to process.
- Working with a DVA advocate like VetComp can make the process clearer, less stressful and more efficient from start to finish.
Understanding the MRCA Claims Process
The Role of DVA
DVA is responsible for assessing and processing compensation claims under the MRCA. Its role includes:
- Determining whether an injury or illness is linked to military service.
- Assessing the level of impairment and eligibility for compensation.
- Providing support services such as rehabilitation and income support.
Types of MRCA Claims
The MRCA covers several different types of claims, including:
- Initial Liability Claims (ILC)– These establish whether a veteran’s injury or illness is service-related.
- Permanent Impairment (PI) Claims – Compensation for long-term disabilities resulting from service.
- Medical Treatment Claims – Requests for specific treatments or healthcare services.
- Income Support and Incapacity Payments – Financial support for veterans unable to work due to their conditions.
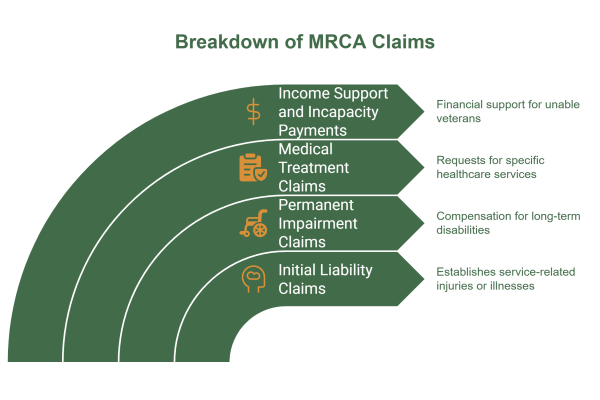
Each claim type has a different level of complexity, which affects how long it takes to process. If you are struggling to know where to go from here, book a free consultation with a VetComp DVA advocate and we can assist you with your claims.
The Importance of Complete Documentation
One of the most common reasons for delays in MRCA claims is incomplete or missing documentation. A successful claim requires:
- Medical evidence – Reports from doctors and specialists confirming the diagnosis and impact of the condition.
- Service records – Proof that the injury or illness is linked to military service.
- Personal statements – Supporting evidence detailing how the condition affects daily life.
Claims that are lodged with all necessary documents upfront tend to be processed more quickly, while those missing key information often face significant delays. When you work with one of our advocates, we ensure that you have or attain all the documentation required, taking the pressure off of you to make sure you have everything. Our team manages this for you, so you’re not left chasing paperwork.
Average Processing Times for MRCA Claims
Processing times for claims vary depending on the type of claim, the complexity of the case, and the availability of required documents. While wait times have historically been lengthy, DVA has made improvements in recent years to reduce delays.
a. Initial Liability (IL) Claims
Initial Liability claims determine whether a veteran’s condition is linked to their service. These claims have historically taken an average of 296 days to process. This includes:
- 70 days from lodgement to officer allocation.
- 226 days from allocation to a decision.
However, processing times have significantly improved. For claims received within the past 12 months, the average processing time has been reduced to 100 days.
b. Permanent Impairment (PI) Claims
Permanent Impairment claims assess compensation for veterans who have sustained lasting disabilities due to their service. These claims take an average of 227 days, including:
- 47 days from lodgement to allocation.
- 181 days from allocation to decision.
While improvements in processing efficiency have helped to reduce delays, certain factors can still affect individual claim timeframes, and claims can take longer or shorter than these averages. At VetComp, our average timeline from signing on board with us to the determination of your PI claims is just under 12 months. Let us advocate on your behalf and take the stress out of DVA claims, book in your free consultation today.
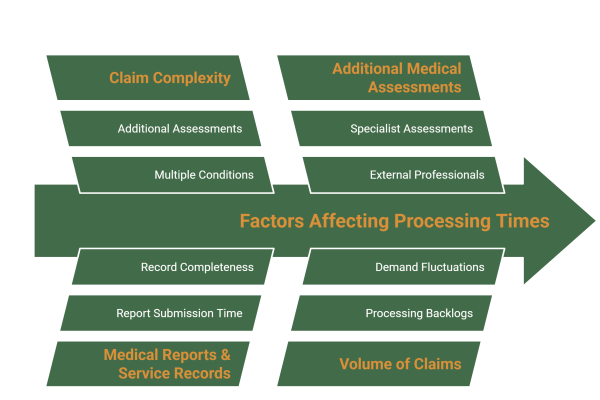
Factors Affecting Processing Times
Claim Complexity
The more conditions included in a claim, the longer it takes to process. As of January 2025, the average MRCA claim includes 4.7 conditions, meaning multiple decisions need to be made within a single application. More complex cases often require additional assessments, slowing down the process.
Medical Reports & Service Records
One of the biggest causes of delays in MRCA claims is the time it takes to obtain medical reports and service records. On average, it takes 72 days for medical reports to be submitted. If the required records are missing or incomplete, additional time is needed for follow-ups, further extending the overall processing time.
Additional Medical Assessments
Some claims require specialist medical assessments to determine the severity of a condition. These assessments depend on external medical professionals, meaning wait times can vary significantly. In some cases, veterans may need to undergo multiple evaluations, further lengthening the process. It can be tricky trying to find veteran-friendly GPs and medical professionals; that’s why we connect you with appropriate providers to help streamline this process and lessen delays due to unnecessary medical appointment setbacks.
DVA’s Efforts to Improve Processing Times
DVA has taken significant steps to reduce the time it takes to process MRCA claims. Recognising the impact that long wait times have on veterans and their families, the department has focused on backlog reduction and process improvements to streamline claims handling.
Backlog Reduction
A key milestone in improving efficiency was the clearance of 98% of the claims backlog identified in the Royal Commission into Defence and Veteran Suicide. As of January 2025, the majority of long-standing cases had been resolved, significantly reducing delays for new claims.
New Processing Standards
With the backlog under control, the DVA has shifted to a “business-as-usual” model, ensuring new claims are processed more efficiently. Under the updated standards:
- Claims are registered, screened, and allocated within two weeks of receipt.
- The focus is on streamlining assessment procedures to reduce overall processing times.
These improvements aim to provide veterans with faster access to compensation and support services, helping them navigate the system with greater certainty.
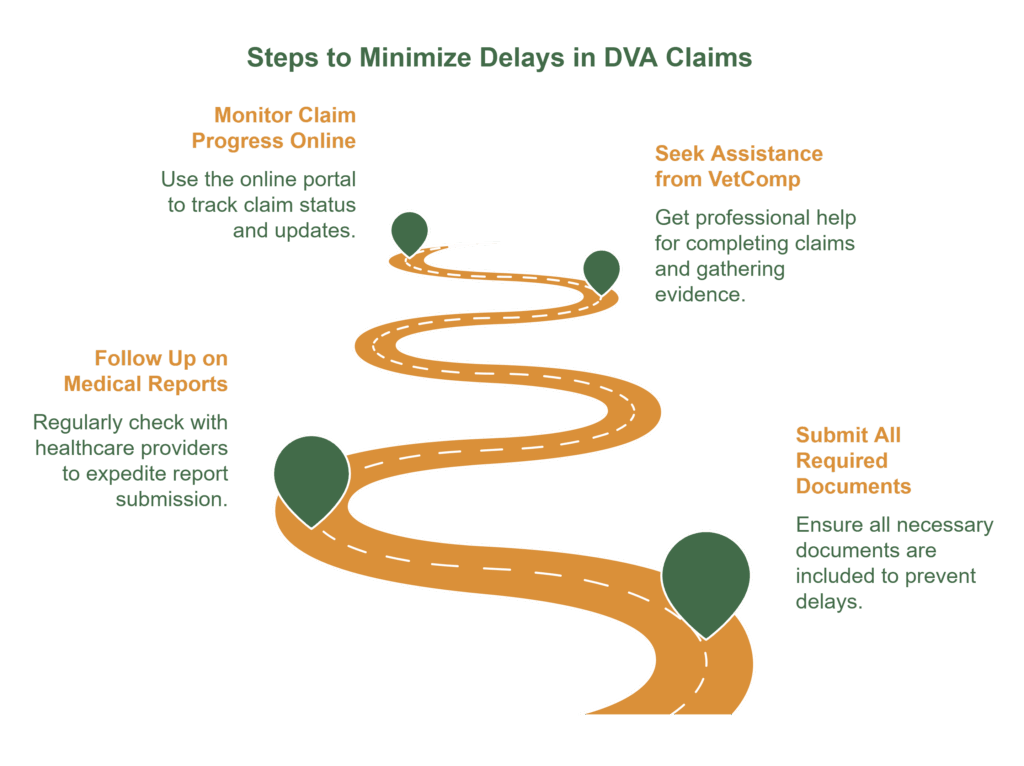
How to Minimise Delays in Your MRCA Claim
While processing times have improved, delays can still occur, particularly when claims are missing important documentation or require additional medical assessments. To avoid unnecessary wait times, veterans should take proactive steps to ensure their claim is processed as smoothly as possible.
1. Ensure All Required Documents Are Submitted
Incomplete applications are one of the most common reasons for claim delays. When lodging a claim, make sure to include:
- Medical evidence (doctor’s reports, specialist assessments).
- Service records (to confirm the link between the condition and military service).
- Personal statements (if applicable, to explain how the condition affects daily life).
2. Follow Up on Medical Report Requests
Medical reports from healthcare providers can take time to be processed—on average, 72 days. To prevent unnecessary delays:
- Request reports as early as possible.
- Follow up regularly with doctors and specialists to ensure reports are submitted promptly.
- Check with DVA if additional information is needed.
3. Seek Assistance from a DVA Advocate at VetComp
Navigating the claims process can be complex, and professional assistance can make a significant difference. VetComp can:
- Help ensure claims are accurately completed.
- Assist with gathering supporting evidence.
- Provide guidance on appeals if a claim is delayed or rejected.
4. Monitor Claim Progress Through DVA’s Online Portal
Veterans can track their claim status through the MyService portal on the DVA website. This allows claimants to:
- Check for updates on their application.
- See if additional documents are required.
- Communicate with claims officers for further assistance.
Additionally, if you are working with VetComp, contact your advocate at any time and they can keep you in the loop as to where your claims are at.
By staying proactive and ensuring all necessary steps are taken, veterans can help minimise delays and speed up the processing of their MRCA claim.
Understanding the MRCA Claims Process and Accessing Support
Navigating the MRCA claims process can be challenging, but having a clear understanding of typical timeframes and what causes delays can help veterans and their families feel more prepared. While wait times have often been lengthy, DVA has made steady progress by clearing most of the claims backlog and introducing new systems to process claims faster.
If you’re about to lodge a claim, being organised makes a big difference. Submitting all required documents early, following up on medical reports, and seeking assistance from a DVA advocate at VetComp can all help minimise delays and improve the chances of a smoother claims process. You can also track your progress through the MyService portal on the DVA website.
If you’re still waiting on a decision, patience matters, but so does having someone on your side. That’s where we come in. We’re here to help you access the support and compensation you’re entitled to, without the added stress.
FAQs
We’ve gathered our most commonly asked questions here, so you can feel informed, at ease, and ready to take the next step toward the support and benefits you deserve.
How long does it take for my claim to be assigned to a case officer?
Under DVA’s new processing standards, MRCA claims are typically registered, screened, and allocated within two weeks of receipt. However, during periods of high demand, this may take slightly longer. Veterans can track their claim’s progress through the MyService portal or contact DVA, or their advocate, for an update.
What happens if additional information is needed for my claim?
If your claim is missing essential documents, such as medical reports or service records, DVA will request further information. This can pause the processing timeframe until the required documents are provided. To avoid delays, veterans should ensure all necessary paperwork is included at the time of lodgement and follow up promptly on any additional requests.
Can I speed up the processing of my MRCA claim?
While processing times depend on the complexity of the claim, veterans can take proactive steps to minimise avoidable delays, including:
- Submitting a complete and well-documented claim.
- Ensuring medical reports and service records are submitted as soon as possible.
- Following up on requests for additional information quickly.
- Seeking assistance from an advocate at VetComp to ensure correct lodgement.
Can I access any interim support while my claim is being processed?
In some cases, veterans may be eligible for interim financial or medical support while awaiting a decision on their MRCA claim. This may include:
- Provisional access to medical treatment (link to our blog about PAMT) for certain conditions.
- Incapacity payments (link to our blog about incap payments) if a veteran is unable to work due to a service-related condition.
- Emergency financial assistance through veteran welfare organisations if delays are causing hardship.
Veterans should contact DVA or their appointed advocate to discuss potential interim support options.
What happens after my MRCA claim is approved?
Once a decision is made, veterans will receive a formal notification outlining:
- The outcome of their claim.
- The compensation amount (if applicable).
- Any ongoing medical or rehabilitation support they are entitled to.
If the veteran disagrees with the decision, they have the right to request a review or appeal. Payments are usually processed shortly after approval, and back payments may be included if applicable.



