“Nearly 60% of women who served in the ADF report having experienced sexual assault or harassment during their military career — and yet their trauma often remains invisible in the compensation process.”
— ADF Service Women Steering Committee Report, 2024
Australia’s female veterans are stepping into the light — but the systems designed to support them haven’t quite caught up. While the number of women serving in the Australian Defence Force (ADF) continues to grow, their unique health needs remain marginalised within the Department of Veterans’ Affairs (DVA) claims and compensation framework. These are not isolated issues; they are systemic gaps that translate into delayed care, misdiagnoses, and inadequate support.
Female-specific health conditions, from reproductive injuries to trauma linked to sexual violence, are often overlooked or poorly addressed in DVA policies and the Statements of Principles (SoPs). Without gender-sensitive frameworks in place, many women face undercompensation and a silence that adds to the physical and emotional burden of their service.
This blog explores how these gaps affect women veterans in real life – the kinds of health conditions they often deal with, the hurdles they face when making claims, and how the system needs to change. It’s time to move past surface-level promises and make sure fairness is built into the policies that are meant to support them.
Key takeaways
- Female-specific health conditions are often under-recognised in DVA policies, leading to gaps in compensation and care.
- Mental health challenges and sexual trauma are more prevalent among female veterans but remain inadequately addressed in claims processes.
- The Statements of Principles (SoPs) lack gender sensitivity, making it difficult for women to have reproductive or hormonal conditions accepted.
- Working with an advocate can improve outcomes, helping veterans access the support, medical evidence, and recognition they deserve.
The Health Burden: Conditions Impacting Female Veterans
The Mental Health Toll
Female veterans face mental health challenges at much higher rates than their civilian peers. Conditions like PTSD, anxiety, and depression are common, often tied to both combat experiences and gender-based trauma. Worryingly, women who’ve served are twice as likely to die by suicide compared to other Australian women.
One major factor is involuntary medical discharge. Being forced to leave due to injury or illness—especially following assault or harassment—can cause deep psychological harm. It takes away more than just a job; it often takes away identity, purpose and community. On top of that, the stigma around asking for help can make things even harder. Sadly, the system still does not do enough to support those most in need.
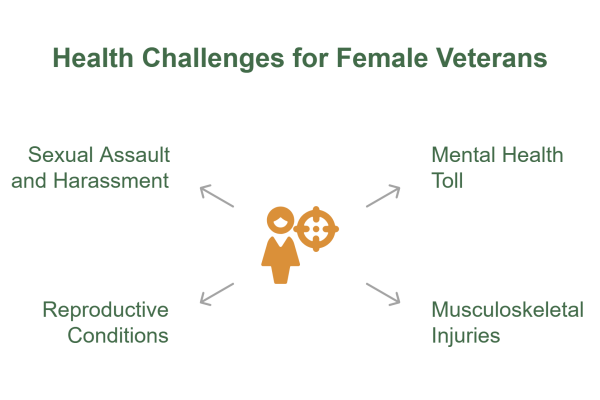
Musculoskeletal conditions are some of the most commonly accepted DVA claims, and female veterans are certainly not exempt. Injuries like lumbar spondylosis, chronic back pain, knee issues and joint sprains often come from the heavy physical demands of service, typically carried out in conditions that don’t account for women’s physiology.
For much of its history, the ADF has relied on male-focused physical training standards. From ill-fitting equipment to a lack of ergonomic support, women have been expected to adjust without any real structural change. Over time, this leads to a higher rate of wear-and-tear injuries—many of which are overlooked or not fairly compensated.
The Hidden Cost of Reproductive and Gynaecological Conditions
Reproductive and gynaecological health still sits in a bureaucratic grey area. Despite being central to many women’s long-term wellbeing, these conditions are poorly represented in the SoPs. There is a category for “Pregnancy, Childbirth, and Puerperium“, but it remains frustratingly empty of practical application.
Menstrual disorders triggered by combat stress and pregnancy complications tied to service conditions aren’t rare or secondary. Reproductive health must be treated as a core part of the conversation. The long-term impact of untreated conditions, including infertility, pelvic pain, and hormonal dysfunction, can affect not just health but also quality of life. Yet too often, women still face barriers to getting these claims recognised, let alone compensated.
Sexual Assault and Harassment in Service
The numbers are confronting. More than half of all female veterans report experiencing sexual harassment or assault during their service. For many, these experiences leave deep psychological scars — PTSD, complex trauma, depression, and anxiety — all made worse by a culture of silence and shame.
Despite the frequency of this trauma, sexual violence remains largely unrecognised within the DVA’s formal compensation frameworks. It is often treated as a peripheral issue rather than a central cause of service-related injury. The absence of structured pathways for recognition and redress not only delays healing, but it also sends a message that the system was never built for women.
📩 Our advocates at VetComp connect you with veteran-friendly medical providers, for both your physical and mental wellbeing, who understand not only the DVA system but also the ADF and its environment.
Roadblocks in the Claims Process: When the System Doesn’t See You
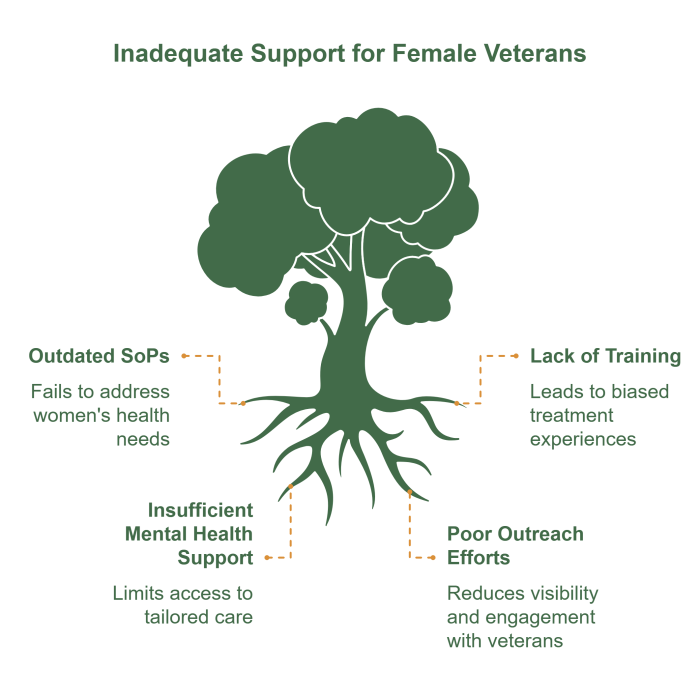
Gender-Blind Policy Frameworks
At the heart of the DVA’s assessment model are the Statements of Principles (SoPs) — medical and scientific guidelines used to determine whether a condition is connected to military service. But here’s the problem: these policies were developed around a predominantly male veteran population. As a result, they often fail to reflect the biological realities of women.
Take, for example, the SoP category for “Pregnancy, Childbirth, and Puerperium” — it exists, but offers little in the way of practical guidance. Conditions like endometriosis, which are worsened by stress, hormonal imbalances, and service-related reproductive trauma, remain largely invisible in this framework. The result? Real conditions get missed, left without support or compensation.
Identity Erasure and the Veteran Label
Too many female veterans report a common refrain: “I don’t feel seen.” Their identities as veterans are often dismissed, whether at the GP’s office, within institutional systems, or even within veteran peer networks. This sense of erasure can fuel internalised doubt, making it harder for women to advocate for themselves when it comes to accessing entitlements.
The cultural narrative around the “veteran” has long been shaped by male experiences — combat, injury, and a visible post-service trajectory. For women, whose injuries may be internal or compounded by sexual trauma, this invisibility becomes a barrier.
When the system itself doesn’t validate your service, how do you begin to claim compensation?
With a VetComp advocate on your side, the process will be smooth as they take the heavy lifting off your hands.
Send us your details, and someone from our team will be in contact
Limited Avenues for Unique Compensation
The current compensation system is rigid. It was built to account for lost limbs, not the kinds of injuries that affect many women, like infertility after service, mastectomies caused by service-related conditions, or long-term pelvic floor damage.
Permanent Impairment assessments, which help decide compensation payments, often fail to reflect the personal and emotional toll of these experiences. A mastectomy, for example, might be viewed only as a physical change, without considering the psychological and identity-related impact it can have. This gap between lived experience and how it’s measured shows that we don’t just need inclusion — we need real change.
The Compensation Frameworks: What’s on Paper vs. What’s in Practice
Military Rehabilitation and Compensation Act (MRCA)
Introduced in 2004, the MRCA is the cornerstone of modern DVA claims. It covers service-related injuries, illnesses, and deaths that occurred after 1 July 2004, providing access to rehabilitation, permanent impairment payments, and household support.
While MRCA does offer a more integrated model compared to its predecessors, it remains imperfect in addressing the nuanced needs of female veterans. Conditions like PTSD and musculoskeletal injuries are well-covered, but female-specific conditions, particularly those tied to reproductive or sexual health, are not consistently recognised or fairly assessed.
The Gold Card: A Healthcare Lifeline?
The DVA Gold Card provides full, cost-free healthcare for veterans with accepted conditions. Once a veteran reaches 60 Permanent Impairment (PI) points, they’re eligible for treatment of all health conditions, even those not officially accepted as service-related. It’s an essential safety net — but for many women, reaching the 60-point threshold is challenging. When female-specific conditions aren’t properly recognised or assessed, it limits access to the care they need and deserve.
This is why working with an advocate at VetComp, who has access to veteran-friendly medical providers with expertise in DVA, can be beneficial. Let your advocate fight on your behalf, ease the burden on yourself.
Rewriting the Narrative: Policy and Practice Recommendations
It’s time to redesign a system that sees, hears, and supports female veterans, not as an afterthought, but as a priority. The current framework, while evolving, still falls short. Here’s what needs to happen next:
Update the SoPs
The SoPs must reflect the real medical experiences of women. That means formally including conditions related to reproductive health, hormonal disruption, sexual trauma, and postnatal complications. This update should be informed by contemporary research and lived experience, rather than outdated clinical models that overlook gendered health outcomes.
Cultural Competency Training
DVA personnel, healthcare providers, and claims assessors must undergo comprehensive gender-awareness training. This isn’t about ticking a box; it’s about transforming how female veterans are treated the moment they walk through the door. Recognising bias, validating trauma, and acknowledging invisible injuries are all essential components of care.
Integrated Mental Health Support
Mental health care must be accessible, stigma-free, and tailored. This includes trauma-informed counselling, options for female practitioners, and programs that connect veterans with advocates who have lived experience. Mental health support should not only treat the wound, it should validate the cause.
Targeted Outreach
Visibility is power. Outreach programs must actively engage with female veterans through community groups, online platforms, and veteran-focused events. Campaigns should affirm that “Yes — your service counts. And yes — your injuries matter.” Only then can we begin to repair trust and rebuild engagement.
Claiming Space, Demanding Change
Australia’s female veterans have carried out their service with strength, commitment, and resilience. But once that service ends, too many find themselves navigating a system that doesn’t fully recognise their sacrifice — or their needs. From overlooked injuries to under-assessed trauma, the path to fair compensation remains uneven.
Female-specific health conditions are not niche or exceptional. They are part of the lived reality of many who’ve served, and they deserve to be treated with the same seriousness and clarity as any other service-related condition. The current compensation framework still has a long way to go — but with stronger advocacy, updated policies, and better cultural awareness, meaningful change is possible.
At VetComp, we’re here to help you be seen and supported. Whether you’re dealing with complex conditions, a rejected claim, or simply don’t know where to start, our advocates are here to lighten the load and walk beside you.
To explore more, you can visit the resources that shaped this blog, including the Women Veterans 2025 Baseline Data Report and the 2024 Female Veterans Policy Forum. The need for change is clear, and the moment to act is now.
FAQs
We’ve gathered our most commonly asked questions here, so you can feel informed, at ease, and ready to take the next step toward the support and benefits you deserve.
I don’t feel like a “typical” veteran — am I still eligible for DVA support?
Yes. If you serve or served in the ADF, you are a veteran — regardless of your role, rank, deployment history, or gender. Your experiences are valid, and you are entitled to seek support, treatment, and compensation through the DVA.
Can I make a claim for conditions related to reproductive or gynaecological health?
Yes, but this area is currently underdeveloped within DVA frameworks. While reproductive health conditions are often harder to claim due to a lack of clear Statements of Principles (SoPs), it is possible — especially with strong medical evidence. VetComp can help you navigate this process and build a robust claim.
I experienced sexual harassment or assault during service. Can I claim compensation for that?
Yes. If the psychological or physical effects of harassment or assault are impacting your health (e.g. PTSD, anxiety, chronic pain), you can claim for service-related conditions. Claims of this nature require sensitivity and support — VetComp can guide you through it with confidentiality and care.
What if my claim has already been rejected?
You have the right to request a review or appeal. Many claims are initially rejected due to missing information, poor documentation, or misinterpretation. With proper support, you can challenge the decision. VetComp advocates can assist in cases of claim reassessments and appeals.
Are mental health conditions like PTSD, depression, or anxiety covered under DVA?
Yes. Mental health conditions are among the most commonly accepted claims — particularly when they stem from service-related trauma, deployments, or military culture. If you’re struggling, you’re not alone, and help is available.
Can I still claim compensation if I left the ADF years ago?
Absolutely. There’s no expiry date for seeking support for service-related conditions. Whether your injury surfaced recently or has worsened over time, you can lodge a claim.
How can VetComp help me?
VetComp is dedicated to supporting veterans — especially those who have felt unseen or unheard in the claims process. We offer personalised guidance on DVA claims, referrals to veteran-friendly medical providers, assistance with appeals, and advocacy every step of the way. Our goal is to help you get the recognition and compensation you’re entitled to, without the stress of doing it alone.



