Understanding Insomnia Among Veterans
Insomnia is a pervasive and often debilitating condition affecting a significant number of Australian veterans. Characterised by persistent difficulties in falling asleep, staying asleep, or achieving restorative rest, insomnia can have profound consequences on mental and physical health. For veterans, sleep disturbances are not merely an inconvenience but a serious health concern that can exacerbate conditions such as Post-Traumatic Stress Disorder (PTSD), depression, and chronic pain.
Understanding the root causes of insomnia in veterans is crucial to developing effective interventions. Military service often exposes personnel to high-stress environments, irregular sleep schedules, and traumatic experiences—all of which can contribute to long-term sleep disturbances. Additionally, transitioning to civilian life can pose its own challenges, with many veterans struggling to establish a stable routine and cope with the psychological effects of their service.
Key takeaways
- Insomnia is common and complex in Australian veterans, often linked to PTSD, chronic pain, and the challenges of transitioning to civilian life.
- Sleep issues can severely impact mental health, physical well-being, and daily functioning, increasing the risk of depression, anxiety, and long-term health conditions.
- Effective treatment includes a combination of therapies, such as Cognitive Behavioural Therapy for Insomnia (CBT-I), sleep hygiene practices, medical support, and lifestyle changes.
- Veterans may be eligible for compensation under MRCA if their insomnia is connected to their service, with support available to guide them through the claims process.
What is Insomnia?
Insomnia is a common sleep disorder characterised by difficulties initiating or maintaining sleep, waking up too early, or experiencing non-restorative sleep. Chronic insomnia, which persists for at least three nights per week over a period of three months or more, can lead to significant impairment in cognitive function, emotional regulation, and overall well-being.
Symptoms of insomnia include:
- Difficulty falling asleep despite feeling tired.
- Frequent awakenings during the night.
- Waking up too early and being unable to fall back asleep.
- Daytime fatigue, irritability, and difficulty concentrating.
For Australian veterans, insomnia often manifests alongside other conditions such as PTSD, anxiety, and chronic pain, making it more challenging to treat and manage effectively. Veterans experience higher rates of insomnia compared to the general population due to the unique demands of military service.
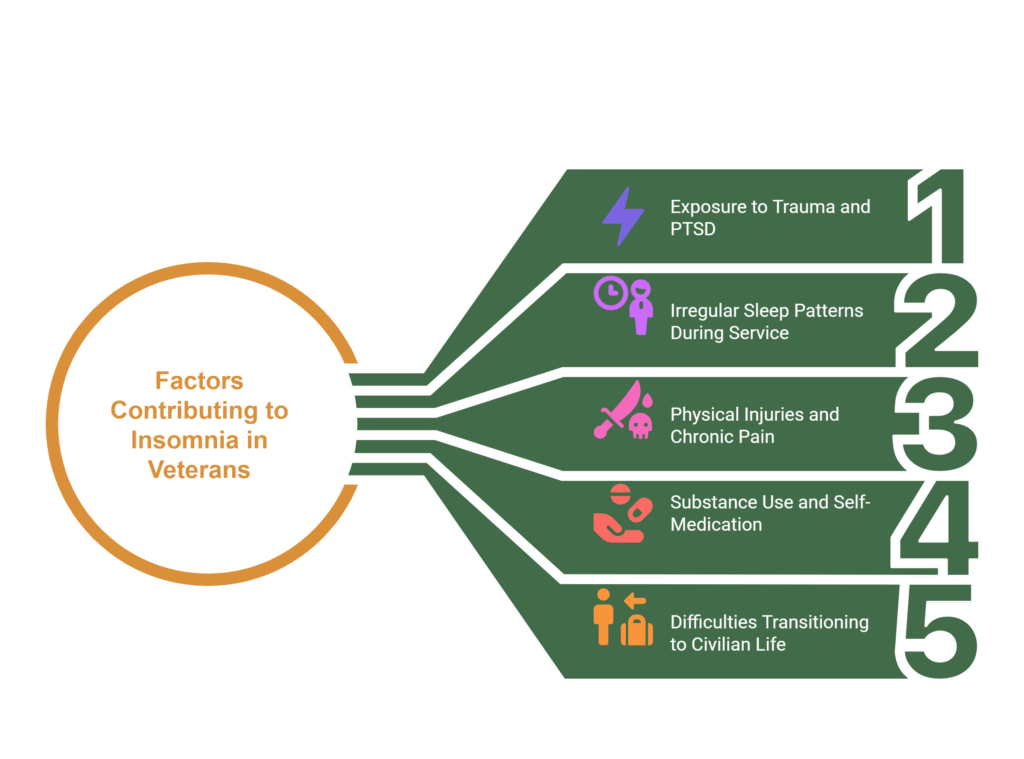
Several factors contribute to this heightened risk:
- Exposure to trauma and PTSD.
- Irregular sleep patterns during service.
- Physical injuries and chronic pain.
- Substance use and self-medication.
- Difficulties transitioning to civilian life.
Causes of Insomnia in Australian Veterans
Insomnia among Australian veterans is a complex issue influenced by multiple factors, including trauma, physical health conditions, military lifestyle, and the challenges of transitioning to civilian life. Understanding these causes is essential to developing effective interventions and support systems.
Trauma and PTSD
A significant contributor to insomnia in veterans is PTSD, a condition that arises from exposure to traumatic events during service, including combat, life-threatening situations, and witnessing distressing incidents. Research has established a strong link between PTSD and sleep disturbances, with insomnia often serving as a core symptom.
Symptoms of trauma and PTSD include:
Hyperarousal and sleep disruptions
PTSD triggers a heightened state of alertness, making it difficult for veterans to relax and fall asleep. Their nervous system remains in a “fight-or-flight” mode, leading to fragmented and poor-quality sleep.
Nightmares and night terrors
Many veterans with PTSD experience recurrent distressing dreams related to traumatic events, causing frequent awakenings and reinforcing a fear of sleep. This cycle often leads to sleep avoidance, further exacerbating insomnia.
Sleep fragmentation
PTSD can cause veterans to wake up frequently throughout the night, preventing them from achieving deep, restorative sleep. Over time, chronic sleep deprivation worsens PTSD symptoms, creating a vicious cycle.
👉 See our page about PTSD information and potential compensation you may be eligible for.
Physical Health Conditions
Many veterans experience long-term physical health issues as a result of their military service, which can significantly impact sleep quality.
Physical symptoms
Chronic pain and sleep disturbances
Service-related injuries such as musculoskeletal pain, arthritis, and nerve damage can make it difficult to find a comfortable sleeping position, leading to frequent awakenings. Pain disrupts deep sleep stages, preventing full physical and cognitive restoration.
Obstructive sleep apnoea (OSA) and PTSD connection
Veterans, particularly those with PTSD, are at a higher risk of developing OSA, a condition where breathing repeatedly stops and starts during sleep. Studies indicate that the combination of PTSD and OSA leads to more severe sleep disturbances, cognitive impairment, and an increased risk of cardiovascular disease. Many veterans remain undiagnosed due to overlapping symptoms of fatigue and irritability with PTSD. Your VetComp advocate can connect you with veteran-friendly practitioners in order for you to get a diagnosis.
Lifestyle and Military Service Factors
Military service exposes personnel to demanding work conditions, which can disrupt normal sleep patterns and persist long after their service ends.
Irregular sleep schedules and shift work
Military operations often require personnel to stay awake for extended periods or sleep in short, fragmented bursts. Over time, this disrupts the body’s natural sleep-wake cycle, making it difficult to establish a regular sleep routine post-service.
Frequent deployments and environmental stress
Deployments often involve sleeping in high-stress, noisy, or uncomfortable environments, contributing to long-term sleep deprivation.
Substance use and sleep disruptions
Many veterans turn to alcohol or medications (including sedatives or stimulants) to regulate their sleep. While these substances may initially provide relief, they often worsen insomnia in the long run by altering sleep architecture and increasing dependence.
Challenges in Transitioning to Civilian Life
Adjusting to civilian life presents significant emotional and psychological challenges, many of which can disrupt sleep patterns.
Loss of routine and structure
Military life follows a highly structured daily routine, with strict schedules for waking, working, and sleeping. The sudden shift to civilian life—where veterans must create their own routine—can lead to sleep disturbances.
Identity shifts and emotional adjustment
The transition from soldier to civilian can be disorienting, leading to anxiety, stress, and a sense of loss, all of which contribute to sleep difficulties.
Work, financial, and social stressors
Finding employment, managing finances, and reintegrating into civilian social circles can create additional stress, further exacerbating insomnia.
If you are struggling with physical or mental conditions as a result of your service, let us help you get the compensation you deserve. Book a free consultation with our team today.
Prevalence of Insomnia Among Australian Veterans
Research consistently shows that veterans experience higher rates of insomnia compared to the general population.
Statistics on insomnia in veterans
- A 37% prevalence rate of sleep disturbances has been reported among U.S. veterans, with 11.4% screening positive for clinical insomnia and 26% experiencing subthreshold insomnia.
- Australian Vietnam veterans with PTSD exhibit significantly higher rates of sleep disorders than trauma-matched controls without PTSD, including restless legs syndrome, parasomnias, and OSA.
Differences between veterans with and without PTSD
- Veterans diagnosed with PTSD are far more likely to experience chronic and severe sleep disturbances compared to their non-PTSD counterparts.
- Research suggests that sleep issues in PTSD-affected veterans often persist for years after leaving the military, unlike in non-PTSD veterans where sleep disturbances tend to decline over time.
Comparison with the general population
- In contrast, only 10-15% of the general adult population experiences chronic insomnia, highlighting the disproportionate burden on veterans.
The Role of Military Service in Long-Term Sleep Disturbances
The effects of military service on sleep can extend well beyond active duty. Veterans often struggle with hypervigilance—remaining in a heightened state of alertness even in safe environments. This can make it difficult to relax and fall asleep, as the brain remains primed for potential threats.
Additionally, studies indicate that conditions like Obstructive Sleep Apnoea (OSA) are more prevalent among veterans, particularly those with PTSD. OSA leads to repeated interruptions in breathing during sleep, resulting in poor sleep quality and daytime fatigue.
By understanding the complex relationship between military service and insomnia, we can better address the sleep challenges faced by Australian veterans and provide targeted support and treatment options. If you are facing insomnia, PTSD, or another condition as a result of your service, you may be entitled to compensation. Reach out to one of our experts to find out more about how we can assist you.
Health Impacts of Insomnia in Veterans
The consequences of chronic insomnia extend beyond sleep deprivation, affecting mental health, physical well-being, and daily functioning.
Mental Health Consequences
Insomnia significantly increases the likelihood of developing or worsening depression and anxiety disorders, particularly in veterans already struggling with PTSD. The frustration of persistent sleep disturbances often contributes to feelings of hopelessness and emotional instability. Additionally, studies indicate that veterans suffering from chronic insomnia are at an increased risk of suicidal thoughts and behaviours. A lack of restorative sleep amplifies emotional distress, reducing the ability to cope with trauma and stress.
Physical Health Risks
Chronic sleep deprivation can lead to serious physical health complications, many of which are already prevalent in the veteran population.
Chronic pain and sleep deficiency
Veterans with insomnia frequently experience heightened pain sensitivity, making conditions such as arthritis, fibromyalgia, and back pain even more difficult to manage.
Hypertension and Cardiovascular Disease
Sleep deprivation is associated with an increased risk of high blood pressure, heart disease, and stroke, particularly in veterans with PTSD and OSA.
Obesity and metabolic dysfunction
Poor sleep disrupts metabolism, increasing the likelihood of weight gain, diabetes, and obesity, which further worsens sleep quality.
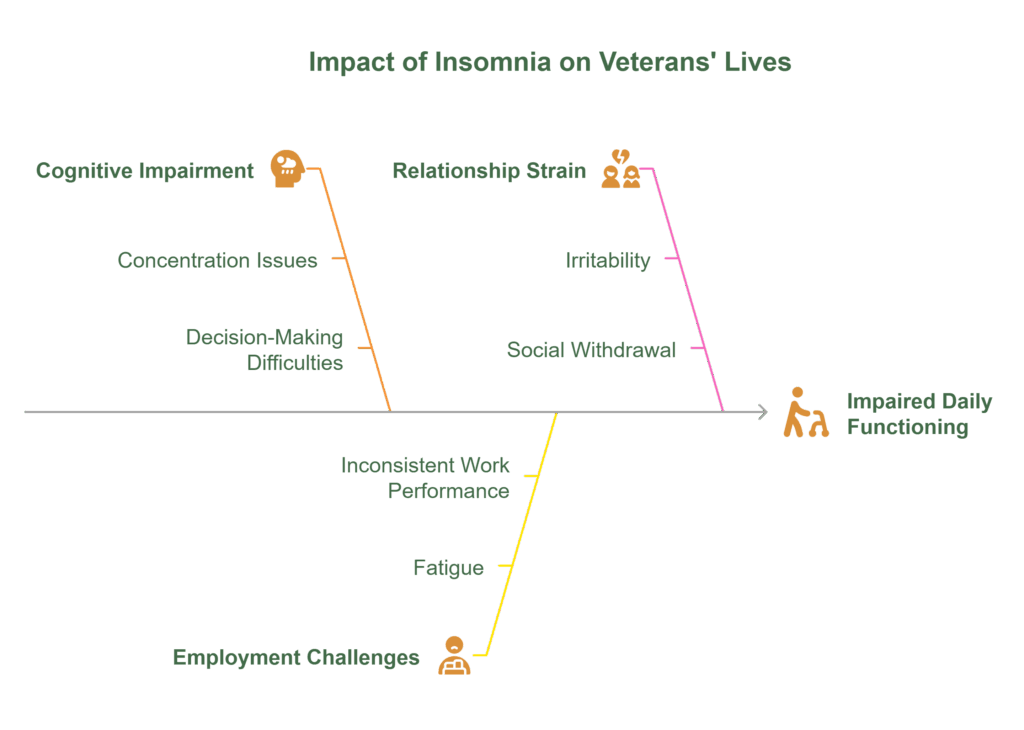
Effects on Daily Functioning
Beyond its impact on health, insomnia can impair veterans’ ability to function effectively in their daily lives.
Reduced cognitive function and memory issues
Sleep deprivation affects concentration, decision-making, and problem-solving skills, making it harder to perform well in work and social settings.
Struggles with employment and productivity
Many veterans with chronic insomnia report difficulties maintaining consistent employment, as fatigue and cognitive impairment hinder their ability to meet workplace demands.
Impact on relationships and social engagement
Poor sleep can lead to irritability, mood swings, and social withdrawal, straining relationships with family and friends.
By recognising the serious health implications of insomnia, it becomes clear that targeted intervention and support are essential to improving the well-being of Australian veterans. The VetComp team can assist in connecting you with appropriate support during and after pursuing DVA claims you may be eligible for.
Treatment and Management Strategies
Effectively managing insomnia in Australian veterans requires a multifaceted approach that addresses both psychological and physiological factors. While some veterans may benefit from professional medical interventions, others find relief through behavioural strategies, lifestyle modifications, and improved sleep hygiene.
Cognitive Behavioural Therapy for Insomnia (CBT-I)
Cognitive Behavioural Therapy for Insomnia (CBT-I) is widely recognised as the gold-standard treatment for chronic sleep disorders. Unlike medications, which only provide temporary relief, CBT-I targets the root causes of insomnia by helping individuals modify negative thought patterns and behaviours that disrupt sleep.
For veterans, CBT-I is particularly effective in breaking the cycle of PTSD-related sleep disruptions, including nightmares and anxiety-induced insomnia. Programs tailored to veterans may integrate trauma-focused therapy alongside CBT-I to maximise its benefits.
Sleep Hygiene Best Practices
Developing healthy sleep habits—often referred to as sleep hygiene—is a critical component of managing insomnia. Small adjustments in daily routines can significantly improve sleep quality and promote long-term wellness.
Establish a consistent sleep routine
- Develop a relaxing pre-bedtime routine, such as reading or meditation.
- Wake up and go to bed at the same time every day, even on weekends.
Optimise the sleep environment
- Keep the bedroom cool, dark, and quiet to minimise disturbances.
- Invest in a comfortable mattress and pillows to reduce physical discomfort.
Reduce stimulants before bedtime
- Avoid caffeine, nicotine, and alcohol at least four hours before sleep.
- Minimise screen time (phones, TVs, and tablets) as blue light suppresses melatonin production.
For veterans struggling with sleep disorders, following a structured sleep hygiene plan in combination with therapy can enhance treatment outcomes.
Professional Support and Medical Interventions
While behavioural therapies and sleep hygiene improvements are beneficial, some veterans require professional intervention to diagnose underlying medical conditions and determine appropriate treatment options.
Polysomnography Assessments (Sleep Studies)
- Veterans experiencing severe sleep disturbances, chronic fatigue, or suspected OSA may undergo a sleep study to assess brain activity, breathing patterns, and sleep quality. This test is critical in diagnosing sleep disorders beyond primary insomnia, including PTSD-related nocturnal arousals.
Medications for Sleep Disorders
- In some cases, short-term use of sleep aids such as melatonin, sedative-hypnotics, or antidepressants may be prescribed. However, prolonged use of sedatives like benzodiazepines or Z-drugs is generally discouraged due to dependency risks and side effects (e.g., daytime drowsiness, memory impairment).
Veterans should always consult a medical professional before starting or stopping any sleep medication, as misuse can worsen insomnia in the long run. Ask your advocate about connecting you with the necessary medical support team, to ensure you are getting the care you deserve.
Exercise and Lifestyle Adjustments
Regular physical activity plays a crucial role in managing stress, anxiety, and sleep quality. Studies indicate that moderate-intensity exercise can significantly improve sleep duration and efficiency.
Recommended activities for veterans include:
- Low-impact activities like yoga, swimming, or cycling can help reduce stress and promote relaxation.
- Strength training and cardiovascular exercises contribute to better sleep efficiency and reduced symptoms of PTSD.
- Avoid exercising too close to bedtime, as intense workouts can elevate cortisol levels, making it harder to fall asleep.
Lifestyle changes, including reducing alcohol intake, managing stress levels, and fostering a healthy diet, also support long-term sleep improvement.
Compensation for Insomnia Under the Military Rehabilitation and Compensation Act (MRCA)
Veterans whose insomnia is linked to military service may be eligible for compensation under MRCA. This legislation provides financial and medical support for current and former members of the Australian Defence Force (ADF) suffering from service-related conditions.
Understanding MRCA and Veteran Entitlements
MRCA covers veterans whose medical conditions, including insomnia, PTSD, and related sleep disorders, are directly linked to their service. Key provisions include:
- Access to medical treatment and rehabilitation services.
- Financial compensation for those whose conditions impact their ability to work.
- Permanent impairment payments for veterans with long term disabilities.
👉 See our page about MRCA and compensation you may be eligible for.
Eligibility Criteria for Insomnia Claims
To qualify for MRCA compensation, veterans must provide evidence that their insomnia is directly linked to military service. This may include:
- Medical records documenting persistent sleep disturbances.
- Psychiatric or psychological evaluations diagnosing PTSD, anxiety, or depression-related insomnia.
- Service records indicating deployment history, combat exposure, or operational stress.
The strongest claims typically establish a direct link between PTSD, chronic pain, and insomnia, supported by medical assessments and professional testimony. Connect with a VetComp advocate, and they will carry the heavy lifting of your claims. The only thing you have to do is show up to medical appointments, we handle the rest.
The Path to Rest, Relief, and Recognition
Insomnia remains a serious and prevalent issue among Australian veterans, often exacerbated by PTSD, chronic pain, and the transition to civilian life. Left untreated, it can have devastating effects on mental health, physical well-being, and quality of life.
Effective treatment options, including CBT-I, sleep hygiene improvements, professional medical interventions, and lifestyle adjustments, can help veterans manage and reduce sleep disturbances. Additionally, recognising insomnia as a service-related condition under the MRCA ensures that veterans can access the compensation, treatment, and support they deserve.
By raising awareness, providing targeted treatment, and ensuring veterans receive the recognition and assistance they need, we can help those who have served achieve better sleep and a better quality of life.
Let us help you get the compensation and support you deserve.
FAQs
We’ve gathered our most commonly asked questions here, so you can feel informed, at ease, and ready to take the next step toward the support and benefits you deserve.
Why is insomnia more common among veterans than the general population?
Veterans often experience unique stressors during military service, such as irregular sleep schedules, exposure to trauma, and high-pressure environments. These factors—combined with physical injuries and challenges in transitioning to civilian life—contribute to higher rates of insomnia. PTSD, chronic pain, and hypervigilance are particularly strong contributors.
How does insomnia affect my mental and physical health?
Chronic insomnia can worsen conditions like PTSD, depression, and anxiety. It also increases the risk of high blood pressure, heart disease, obesity, and chronic pain. Many veterans report difficulty concentrating, irritability, and poor performance at work or in social settings due to poor sleep.
What are the signs that my insomnia may need professional attention?
If you experience any of the following at least three times a week for more than three months, it may be time to seek help:
- Difficulty falling or staying asleep
- Waking up too early
- Daytime fatigue, irritability, or memory issues
- Frequent nightmares or night terrors
- Reliance on alcohol or substances to sleep
What treatment options are available for veterans with insomnia?
Veterans can benefit from a combination of:
- Cognitive Behavioural Therapy for Insomnia (CBT-I)
- Sleep hygiene education
- Medical treatment, including sleep studies or medication when appropriate
- Lifestyle adjustments, such as regular exercise, stress management, and reduced screen time or alcohol intake
Tailored programs that address PTSD and trauma are often the most effective for long-term improvement.
Can insomnia caused by military service be compensated?
Yes. If your insomnia is connected to your time in the military, you may be eligible for compensation under the Military Rehabilitation and Compensation Act (MRCA). This includes access to:
- Medical and psychological treatment
- Financial compensation
- Permanent impairment payments for long-term effects
VetComp can help assess your eligibility and guide you through the claims process with minimal stress on your part.



